In this interview, Georgi Dinkov, an expert on linoleic acid (LA), details some of the health hazards of this exceedingly common fat in the modern diet, and how to safely rid your body of it.
Both Georgi and I are convinced excessive LA intake is one of the most important variables that can make or break your health, especially in the long term. It’s a far greater contributor to chronic and degenerative disease and mortality than sugar, and it’s the primary culprit that makes processed foods so harmful.
The historical (last 50 to 75 years) incidence curves of cancer, cardiovascular disease (CVD), diabetes and neurological disease in the general population overlap remarkably well the ever-increasing PUFA consumption rates in developed countries, suggesting PUFA is a major factor in those diseases.1,2
How Georgi Became a Biohacker
Despite having a degree in computer science, Georgi has made a name for himself as an expert biohacker. After graduating from college in 2002, he got a job as a programmer at the National Biomedical Research Foundation (NBRF).
There, he helped develop uniprot.org, a database of all known protein sequences — Protein Information Resource (PIR — pir.georgetown.edu) and UniProt (www.uniprot.org).
Surrounded by up to 60 of the brightest doctors and biochemists in the world, Georgi developed an interest in biochemistry, and started studying on the side so he could more effectively collaborate with his coworkers. He provides an amazing example of what one can learn without any formal training if they merely apply themselves.
“Between 2002 and 2005, I was part of this group as a programmer, but I basically started attending all of their lectures and classes,” he says. “Some of them were teaching at nearby universities, so I kept going.
I was a young, single person, didn’t have anything better to do, and I tried to utilize my time the best I could. Over a period of about three years, it started to click, so I started to understand what these people were talking about.
In 2005, I left, got myself a full-time job in the IT sector, and then kept reading. The reason I got into this bioenergetic area, which linoleic acid is a big part of, is because around 2009, I … became a low-carber.
Being an athlete in college, I basically happened to combine very low carb diet with very exhaustive exercise, and I got myself into a really big predicament. I started getting these very weird neurological symptoms, tingling of the extremities, headaches, sensitivity to light.”
Low-Carb Considerations
In the interview, we clear up some of the pervasive confusion surrounding low-carb diets, and why long-term chronic low-carb is not ideal. It’s a great short-term intervention for most people, especially those with insulin resistance.
This is because lowering carbs can help reset your metabolism and recover your metabolic flexibility. However, in the long term you can run into trouble — especially if you’re also doing a lot of endurance training. The main reasons for the issues caused by chronic low-carb diets (and/or stress, which mimics the effects of low-carb diets) are:
- The elevated lipolysis in a low carb-state, which results in chronically elevated circulating levels of PUFA, with the resulting inflammatory and endocrine effects (e.g. PUFA is pro-cortisol, estrogenic and also synergizes with endogenous/exogenous estrogens, and promotes their effects even in low doses).
- The downregulation of the resting metabolic rate (RMR) by lowered synthesis of T3 when eating a low-carb diet and/or fasting and/or strenuous exercise.
For more details on this, be sure to listen to the interview at normal speed. Believe me, this is an interview that nearly everyone should listen to a few times to capture the incredible clinical pearls that Georgi shared. I personally learned more during this discussion than I have from most interviews.
If you listen to the interview, you will learn that once your sugar stores are expended, you start tapping into your fat stores through a process called lipolysis. This liberated fat is then circulated around your body and supplied to the cells as fuel to compensate for the low glucose availability.
However, certain types of fat block the effects of insulin in your body, so a long-distance endurance athlete can actually end up with a blood profile similar to that of a person with Type 2 diabetes. In Georgi’s case, as an endurance athlete, his blood sugar climbed higher the less sugar he ate. This competition/antagonism between glucose and fats (mostly PUFA) as fuel for the cells was first discovered in the 1970s and named the Randle Cycle.
Why does it occur? The process in your liver that controls blood sugar is gluconeogenesis. If you stop supplying carbs to your body, the organs that need them will activate glucose creation in your body by elevating the stress hormone cortisol, which ends up being very destructive to your tissues, including skeletal muscle, liver, brain and kidneys.
In Type 2 diabetes, a state with hyperglycemia, only about 10% of the circulating glucose is of dietary origin. The rest is due to chronically elevated gluconeogenesis — which suggests that cortisol is the driver of hyperglycemia in Type 2 diabetes — and elevating cortisol chronically by doing low-carb or exhaustive exercise is likely detrimental to insulin sensitivity.
People with elevated cortisol (Cushing phenotype) have the same central obesity and loss of muscle mass (sarcopenia) as the ones seen in diabetes 2. Conversely, blocking cortisol’s effects with the drug RU486 has been demonstrated to lead to sustained fat loss WITHOUT dieting, and improved insulin sensitivity.3,4,5
Cortisol goes up during exercise, and if there’s no glucose around, cortisol rises even higher. Shakes, problem sleeping, jitteriness and neurological abnormalities are some of the symptoms of high cortisol and low glycogen stores. In Georgi’s case, his symptoms slowly vanished once he started eating a more balanced diet, with a macronutrient ratio of about one-third carbs, one-third fat and one-third protein.
Dietary Fats and Fatty Liver Disease
In his search for answers to the symptoms he experienced on a low-carb diet, he came across Dr. Peat’s website,6 aka, Dr. T.A. Peterson, an American biologist who’s been studying the role of energy in the cell, and the effects of LA. Georgi started reading Peat’s work in 2009, and eventually started doing his own experiments.
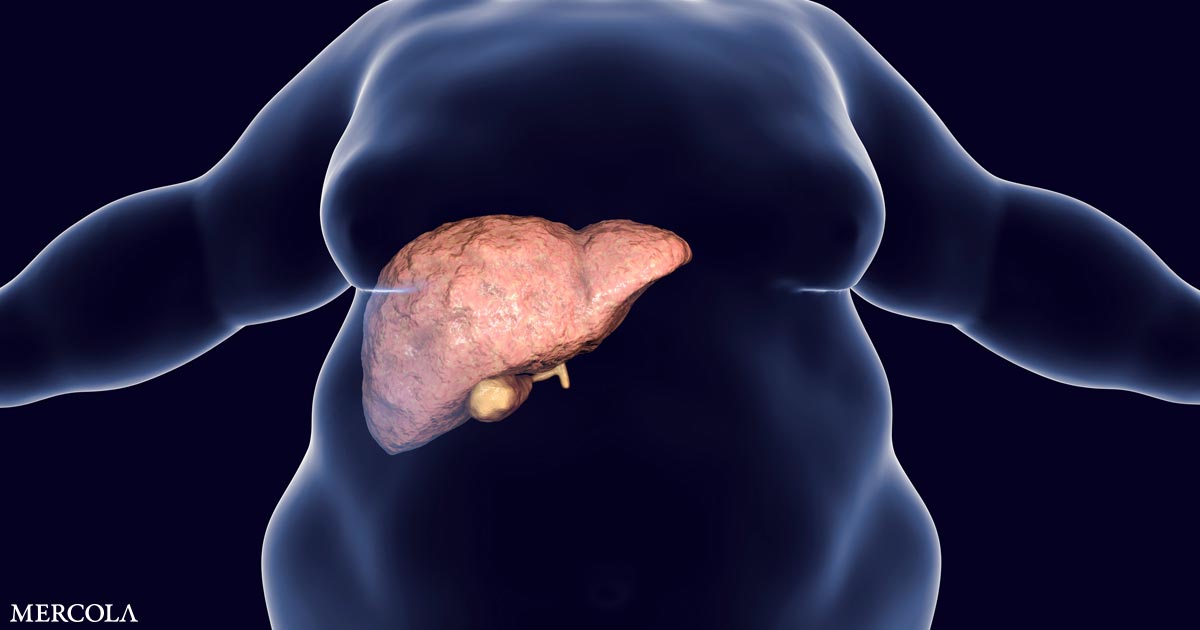
As noted by Georgi, published research has long demonstrated that LA is far from a benign macronutrient. It’s actually a highly proinflammatory mediator and has endocrine effects that mimic estrogen. Contrary to popular belief, LA is also a major culprit in nonalcoholic fatty liver disease (NAFLD), more so than fructose and other sugars.7,8
Georgi cites research9,10,11 showing people with alcoholic cirrhosis (liver disease) who ate their normal diet, which was high in omega-6 fats, experienced classic progression of cirrhosis resulting in liver failure. The group whose diet was altered to eliminate all forms of fat aside from coconut oil, a saturated fat, was able to reverse their cirrhosis, even in the presence of continued alcohol abuse. Additional animal experiments12 confirmed these results. As explained by Georgi:
“The livers of people who are eating predominantly omega-6 fatty acids very quickly get fattened up. Also, there’s cell damage of the Kupffer cells due to the many oxidation byproducts (OxLAMs) of these omega-6 fatty acids … [Meanwhile], the livers of the animals that were still alcoholic but were given the saturated fatty acids had very little oxidative damage to the cells, and they weren’t fat.
What could explain this? Well, it turns out that when you’re consuming a meal with fat, it’s composed of many different fatty acids, but we can separate them into saturated fatty acids, monounsaturated and polyunsaturated [PUFAs].
It turns out that the liver and most of the organs preferentially oxidize (burn) the saturated fatty acids, and then the monounsaturated fatty acids, while the polyunsaturated acids are predominantly stored.
The polyunsaturated fatty acids, aside from being very susceptible to spontaneous auto oxidation … combustion … are precursors to inflammatory mediators such as prostaglandins and leukotrienes. Those inflammatory mediators are basically derived from … linoleic acid. So, if you eat a lot of polyunsaturated fats, and specifically linoleic acid, you’ll have more … systemic inflammation.
Now NAFLD is already known to be an inflammatory state. You cannot get an inflammatory state from saturated fat. It does not produce those same mediators. Saturated fat will either get stored or will get oxidized properly through the process of beta oxidation to carbon dioxide, ATP and water.
But the polyunsaturated fats, they’re unstable. They can get combusted and create a lot of toxic byproducts, and the liver being the site of the primary organ of detoxification of whatever you are eating through the diet — guess what? They’re going to go mostly there.
Also, because they’re precursors to a number of different mediators, enzymes in the body will take these fatty acids, specifically linoleic acid, and then through a chain of reactions convert it to prostaglandins, leukotrienes and thromboxane.”
PUFAs Are Stored, Not Digested
An important take-home here is that PUFAs such as LA are not digested. Instead they’re stored.13 Most of the body fat in obese individuals is composed of PUFAs, not saturated fat. Saturated dietary fat is mostly burned (oxidized) and used up.
So, obese individuals are typically not eating very much saturated fat; rather, they’re exponentially overdosing on LA. Animal studies in the early 20th century demonstrated conclusively that pigs fed saturated fats (mostly coconut oil) could not get fat but became lean and muscular, while the ones fed PUFA gained mostly fat.
This led to the adoption/promotion of PUFA as animal feed since the goal there is to maximize “caloric efficiency” — i.e., get the animals as heavy as possible with a little food as possible. In other words, the pro-obesity effects of PUFA and anti-obesity effects of saturated fats are well-known in the livestock industry and are not disputed.
Considering the similarity of our metabolism/structure/tissues/organs with those of pigs, it should not be at all surprising that we keep getting fatter while consuming ever-larger amounts of PUFA.
The half-life of PUFAs such as LA, which get embedded and integrated into your cell membranes, is about 680 days. This means that to rid your body of LA will take approximately seven years, provided you don’t load more in. And you really do want to get rid of this fat, as it’s highly inflammatory and prevents your mitochondria and cellular machinery from operating properly.
Research has shown that given enough PUFAs, your cells will go into apoptosis, they basically commit suicide. “It can actually work like a radiation or chemotherapy. It is a type of chemotherapy,” Georgi says. The implications14,15 of this insight are quite profound and I look forward to exploring that with Georgi on his next interview.
PUFAs Coming Out of Storage Can Cause Trouble
A key way to eventually lower your body burden of LA is to keep your total LA intake below 2%, maybe even close to 1%. You need to stop putting more in. Exercise and fasting will help drive the LA out, but you need to be really careful if you have a lot of LA storage.
“A recent study16 found that even lean people who are running marathons, a good portion (82%!) of them are actually in acute kidney failure by the time they reach the finish line,” Georgi says. “The question is, how is this possible? It looks like these circulating fatty acids, which are mostly PUFAs coming out of storage, circulate and cause energetic problems.
Also, because of the quick peroxidation and conversion into inflammatory mediators, they’re damaging many of the organs, predominantly the kidneys.17 Why the kidneys? Anything that is not oxidized for fuel basically gets sent to the liver through the blood stream, the Phase 2 detoxification mechanism. The liver attaches glucuronic acids to these fatty acids to make them more water soluble.
It can also sulfate them. When they’re more water soluble, you pee them out. But they have to go through the kidneys, and it looks like if a sufficiently big supply of these glucoronidated sulfated PUFAs, or let’s say linoleic acid just for the sake of the argument, is flooding the kidneys, it is causing local damage there.
So, what should we do? Well, it looks like we should be taking measures to not get into excessive lipolysis. What is excessive lipolysis? It’s any situation where you’ve run out of glycogen and now the body says, ‘I don’t have the fuel,’ because you’re not eating and you’ve run out of glycogen.
Then fat is your only other fuel, plus the amino acids that are coming from cortisol. So basically, you should not be getting to a state where you’re chronically starving. Acute, let’s say like eight to 12 hours of fasting, calorie restriction, has been shown to have benefits, but anything longer than that, then you’re starting to increase baseline lipolysis.”
My Recommendations for TRE Have Changed
Georgi pointed out the dangers of an excessive time-restricted eating (TRE) window.18,19,20,21,22,23,24,25 An extreme example of TRE is the one meal a day (OMAD) protocol, where you’re fasting 20 hours or more each day. Georgi believes this is too extreme for most people, as most have large stores of LA that need to be purged safely.
I have been personally practicing and advocating a six– to eight-hour time restricted eating window. What I learned from our conversation is that this, or even longer eating restrictions and fasts, are perfectly appropriate for 95% of the population as they are insulin resistant and metabolically inflexible.
The major problem comes once you lose your insulin resistance and become metabolically flexible. At that point, this strategy becomes counterproductive as you will increase your cortisol levels, which causes chronic inflammation that can lead to tissue damage. Usually, it takes about three to six months for you to recover your metabolic flexibility.
Prior to my interview with Georgi I would have a six- to eight-hour eating window and I did this for a few years. Now I am going to shift to one day a week of 12 hours, three days of 10 hours and three days of eight hours. If you are metabolically healthy, I would encourage you to avoid very short eating windows under eight hours.
This is because chronic fasting also elevates your cortisol, just like chronic endurance exercise does. Cortisol, in turn, is involved in insulin resistance and the synthesis of fat, and promotes the storage of fat. Also, as just mentioned above, high amounts of LA can kill your cells.
“So, you don’t want to be doing this to your normal tissues, and you’re doing it to your tissues every single time you over-exert yourself to the point of either glycogen running low or you’re so stressed that your adrenaline has gotten to the point where it’s increasing lipolysis and you’re starting to shed fat.”
This is a massive piece of the puzzle that I never fully appreciated. Molecular biology and pH physiology are based on a pre-1860s scenario where you didn’t have these high levels of LA, which totally distorts the strategies. If they weren’t there, you could fast to activate autophagy and get all these benefits.
You could have a much longer TRE window. But LA is a game changer. It radically modifies the concept of what you need to do to optimize your health. Essentially, if you’ve filled up your fat stores with LA — and in most people, over 20% of their fats are LA stored in their cell membranes and the optimum is 1% to 2% — then you need to integrate that knowledge into your strategy.
How to Safely Purge LA
How can you safely reduce these stores of LA without self-sabotaging? As explained by Georgi, extensive fasting will, in this instance, backfire, as will overtaxing yourself with heavy exercise. You’ll need to accept that this is a marathon, not a sprint, and that it’s going to take years to purge your LA stores. The best strategy, Georgi says, is to build muscle and maximize lean muscle mass.
“What does that mean? Concentric exercise, stimulating the muscles to grow. We already mentioned that cortisol is a very catabolic steroid for the muscles, so [you don’t want that] chronically. Acute spikes of cortisol are unavoidable. But things such as chronic fasting or eating inflammatory foods should be avoided as much as possible, which means cutting out vegetable oils.
If you’re cooking your own food, you have the tools at your disposal to eliminate almost completely the consumption of polyunsaturated fats. If you have to fry things or cook on high temperature, use butter, ghee or beef tallow. Even coconut oil [is good], but it has a lower smoke point. All of these are very good substitutes.”
Also avoid all processed foods, restaurant foods, condiments and animal foods raised on grains, such as chicken and pork. Aside from switching the types of dietary fats you eat, Georgi recommends a diet with a 2-to-1 ratio of carbs to protein, the carbs being in the form of fruits and vegetables, not processed sugary snacks.
“Protein is thermogenic. It’s going to raise your metabolic rate. It’s important to consume it with enough carbs because one of the quickest ways to damage your kidneys is consuming a very high protein diet without sufficient amount of carbs.
Even a competitive bodybuilder can only fully utilize about 120 grams of protein a day. Everything else that a person consumes is going to get oxidized as fuel and in the process gets deaminated, which means it produces ammonia, which is very toxic. It destroys the kidneys, liver and brain.
So, eat your protein, don’t cut down on the protein, but don’t overdo it. Make sure the ratio of carbs to protein is at least two to one, and completely cut out PUFAs as much as possible, especially if you’re cooking your own food.”
Hopefully you didn’t skim this and miss the pearl at the end, to take twice as many carbs as protein. What Georgi didn’t state here, though, is that is for people who are metabolically flexible and not insulin resistant.
So, the key is not to be afraid of healthy carbs: They are your friend. If you are eating enough protein to build muscle, please make sure you also have enough carbs because, if you fail to do this, you can hurt your kidneys, liver and brain.
He also shared another pearl about resistance exercises that I wasn’t aware of. Eccentric exercise, in which you are resisting gravity on the way down, builds muscles, BUT it also damages your muscles and destroys the mitochondria. It is far better to focus on the concentric phase of exercise, as it builds more and stronger mitochondria. Concentric exercise increase mitochondrial biogenesis, and steroidogenesis in muscle.26
How PUFAs Cause Heart Disease
Saturated fats improve the structure of cells, specifically the lipid bilayer, while PUFAs like LA impair it. The reason your cholesterol and LDL levels may go up when switching to saturated fats is because you’re giving the cells the structural material needed, from which the cells can synthesize their own cholesterol as needed. Hence, extra cholesterol gets dumped into the bloodstream because it isn’t needed.
Cholesterol is carried around by LDL. So, when you’re eating saturated fat, your LDL rises, but it’s rising because the cholesterol already in the cell is not as needed anymore. It’s actually a good sign.
Conversely, when you’re eating PUFAs, your cells need more cholesterol to strengthen their structure, so your body dumps cholesterol into the cells to protect them from the onslaught of the PUFAs. Hence, it appears your cholesterol level is going down, but it’s actually having a strongly negative effect.
Additionally, the LA becomes oxidized and the LDL carrying it is now oxidized LDL, which is strongly associated with plaque. Plaque, associated with heart attacks also contains white blood cells, calcium, 7-ketocholesterol and PUFA peroxidation byproducts. Saturated fat does not contribute to plaque.
“The plaque is basically a reaction to an inflammation caused by these toxic PUFA byproducts, and PUFA itself is inflammatory. When it gets lodged into the blood vessel walls, it causes a localized inflammatory reaction. The first response of the body is to send white blood cells to protect the blood vessel wall from damage and rupture. That’s really the purpose of the plaque.
So, the body’s not trying to kill you. It’s simply trying to repair in the best possible manner, to isolate the issue. And the issue that it’s trying to isolate is the PUFA peroxidation byproducts27 and 7-ketocholesterol.28 How can you get around this? Don’t eat PUFA, or at least drastically reduce it. Go back to whatever your grandmother was eating.”
Concluding Thoughts
Like me, Georgi is convinced LA is a primary culprit in chronic diseases. And, since LA is found in most whole foods, there’s really never any need to take an omega-6 supplement. It’s virtually impossible to get too little from your diet.
I believe omega-6 supplements really ought to be removed from the market altogether, as people are getting 25 times more omega-6 than they could possibly need from their diet. At most, you need about 2 grams a day, but the average American gets about 50 grams a day, thanks to the fact that most processed foods and condiments are loaded with omega-6 seed oils.
If our diet were to be shifted away from seed oils to saturated fats, the way it was 150 years ago, we’d likely see a massive decline in chronic diseases, including cancer and heart disease.
To learn more, be sure to listen to the entire interview, as we dive into far greater detail than what I’ve summarized here. Georgi is an absolute fire hydrant when it comes to biochemical details. Also check out Georgi’s blog at www.haidut.me. You can also obtain a major sampling of Ray Peat’s work for free by going to these two sites: wiki.chadnet.org/Ray-Peat and RayPeat.com.