
This article was previously published January 1, 2019, and has been updated with new information.
Vitamin D deficiency is incredibly common around the world, but many mistakenly believe they aren’t at risk because they consume vitamin D-fortified foods, such as milk. However, few foods have therapeutic levels of vitamin D naturally, and even fortified foods do not contain enough vitamin D to support your health needs.
Despite its name, vitamin D is actually a steroid hormone that you obtain primarily through sun exposure, not via your diet. Since most dermatologists and other doctors recommend avoiding the sun and using sunscreen before venturing outdoors, vitamin D deficiency has reached truly epidemic proportions around the world.
Unfortunately, while the justification for sun avoidance is that it may reduce your risk of skin cancer, by avoiding sun exposure you risk vitamin D deficiency, which in turn raises your risk for many cancers — not only internal ones but also skin cancer, as well as a whole host of chronic diseases.
Considering the importance of vitamin D for disease prevention, strict sun avoidance is likely doing far more harm than good. The major problem with sun exposure is burning, not overall exposure. And, the easily treatable forms of skin cancer — squamous and basal cell carcinomas — are the ones most likely to form.
Definition of Vitamin D Deficiency
According to research1 published in June 2018, an estimated 40% of Americans are profoundly vitamin D deficient, defined as having a serum (blood) level of vitamin D below 20 ng/mL (50 nmol/L). Sufficiency is defined as having a level of 20 ng/mL or higher.
Calling someone with a vitamin D level of less than 20 ng/ml vitamin D deficient is like calling someone over 400 pounds simply overweight — in both cases a grossly serious understatement.
Seventy-five percent of American adults and teens are deficient in vitamin D when a sufficiency level of 30 ng/mL is used.2 If the sufficiency cutoff were to be moved to 40 to 60 ng/mL, sufficiency rates in the U.S. would likely be in the high 90% bracket.
It’s important to realize that 20 ng/mL has repeatedly been shown to be grossly insufficient for good health and disease prevention and, really, anything below 40 ng/mL (100 nmol/L) should be suspect. For example, research has shown that once you reach a minimum serum vitamin D level of 40 ng/mL, your risk for cancer diminishes by 67%, compared to having a level of 20 ng/mL or less.3
Most cancers occur in people with a vitamin D blood level between 10 and 40 ng/mL (25 to 100 nmol/L), and the optimal level for cancer protection now appears to be between 60 and 80 ng/mL (150 to 200 nmol/L).
Several studies also show that these higher vitamin D levels are protective against breast cancer specifically. Importantly, a 2005 study4 showed women with vitamin D levels above 60 ng/mL have an 83% lower risk of breast cancer than those below 20 ng/mL! I cannot think of any other strategy that can offer that kind of risk reduction.
More recently, a pooled analysis5 published in June 2018 of two randomized trials and a prospective cohort study came to a near-identical conclusion. The objective was to assess whether there are any benefits to having a vitamin D level above 40 ng/mL, as most studies do not venture into these higher levels.
Indeed, mirroring the 2005 findings, women with vitamin D levels at or above 60 ng/mL had an 82% lower incidence rate of breast cancer than those with levels of 20 ng/mL or less. Published research by GrassrootsHealth reveal as much as 80% of all breast cancer incidence could be prevented simply by optimizing vitamin D and nothing else.

Top 5 Signs of Vitamin D Deficiency
The only way to definitively identify vitamin D deficiency is via blood testing. However, there are some general signs and symptoms to be aware of as well. If any of the following apply to you, you should get your vitamin D levels tested sooner than later, and take proactive steps to boost your level into the 60 to 80 ng/mL range:
1. Ongoing musculoskeletal pain and achy bones — According to vitamin D researcher Dr. Michael Holick, whom I interviewed a few years ago, many who see their doctor for aches and pains, especially in combination with fatigue, end up being misdiagnosed as having fibromyalgia or chronic fatigue syndrome.
“Many of these symptoms are classic signs of vitamin D deficiency osteomalacia,6 which is different from the vitamin D deficiency that causes osteoporosis in adults,” Holick told me. “What’s happening is that the vitamin D deficiency causes a defect in putting calcium into the collagen matrix into your skeleton. As a result, you have throbbing, aching bone pain.”
2. Frequent illness/infections — Vitamin D regulates the expression of genes that influence your immune system to attack and destroy bacteria and viruses, so frequent illness and infections of all kinds, including colds and flu, is a tipoff that your immune function is subpar, which likely means you’re low on vitamin D.
3. Neurological symptoms — This includes depression, feeling blue, cognitive impairment, headaches and migraines. In 2006, scientists evaluated the effects of vitamin D on the mental health of 80 elderly patients and found those with the lowest levels of vitamin D were 11 times more prone to be depressed than those who received healthy doses.7
The same study also found low vitamin D was linked to poor cognitive performance. Several other studies8
have also linked vitamin D deficiency with poor mental function, confusion, forgetfulness and difficulty concentrating. Headaches and migraines are also associated with low vitamin D.9,10
4. Fatigue and daytime sleepiness — Studies have linked low vitamin D to persistent fatigue.11,12 In one case, a woman struggling with chronic fatigue, daytime sleepiness (hypersomnia), low back pain and daily headaches was found to have a vitamin D level below 6 ng/mL.
Her symptoms resolved once she raised it to 39 ng/mL.13 Another study14 found women with vitamin D levels below 29 ng/mL were more likely to complain of fatigue than those with levels above 30 ng/mL.
5. Head sweating — According to Holick, a classic sign of vitamin D deficiency is a sweaty head. In fact, physicians used to ask new mothers about head sweating in their newborns for this very reason. Excessive sweating in newborns due to neuromuscular irritability is still described as a common, early symptom of vitamin D deficiency.15
Top 5 Risk Factors for Vitamin D Deficiency
Several factors will influence your risk for vitamin D deficiency, including the following:
- Rarely spending time outdoors and/or always wearing sunscreen — Researchers have noted that vitamin D deficiency is prevalent in adults of all ages who always wear sun protection (which blocks vitamin D production) or limit their outdoor activities.16 The ideal time for sun exposure is between 10 a.m. and 2 p.m., when the UVB rays are present.
- Darker skin — Your skin pigment acts as a natural sunscreen, so the more pigment you have, the more time you’ll need to spend in the sun to make adequate amounts of vitamin D. If you have dark skin, you may need as much as 10 times more sun exposure to produce the same amount of vitamin D as a person with pale skin.
- Being 50 or older — As you get older, your skin doesn’t make as much vitamin D in response to sun exposure. At the same time, your kidneys become less efficient at converting vitamin D into its active form. Older adults also tend to spend more time indoors (i.e., getting even less sun exposure and therefore vitamin D).
- Obesity — Because vitamin D is fat-soluble, body fat acts as a “sink” by collecting it. If you’re overweight or obese, you’re therefore likely going to need more vitamin D than a slimmer person. In one recent study,17 vitamin D deficiency was three times more prevalent in obese individuals.
- Gastrointestinal problems — Since vitamin D is fat-soluble, which means if you have a gastrointestinal condition that affects your ability to absorb fat, you may have lower absorption of fat-soluble vitamins like vitamin D as well. This includes gut conditions like Crohn’s, celiac and nonceliac gluten sensitivity and inflammatory bowel disease.
Health Benefits of Vitamin D Optimization
Optimizing your vitamin D levels has been shown to have a powerful effect on health, helping protect against a wide variety of diseases. Among them:
|
Dry eye syndromes18,19 |
|
Macular degeneration,20,21 which is the No. 1 cause of blindness in the elderly. |
|
Autoimmune diseases — Vitamin D is a potent immune modulator, making it very important for the prevention of autoimmune diseases such as multiple sclerosis, inflammatory bowel disease and psoriasis, just to name a few. |
|
Gastrointestinal diseases22 — Dysbiosis of your gut microbiome, inflammatory bowel disease and colitis are all disorders connected to vitamin D deficiency. |
|
Infectious diseases, including influenza and HIV23,24 |
|
Inflammatory rheumatic diseases25 such as rheumatoid arthritis — A 2020 study showed that “vitamin D supplementation seemed to be an effective intervention for patients with rheumatoid arthritis. Different doses of vitamin D and durations of intervention produce different effects.” |
|
Osteoporosis and hip fractures |
|
Cardiovascular disease — Vitamin D is very important for reducing hypertension, atherosclerotic heart disease, heart attack and stroke, as it plays a vital role in protecting and repairing damage to your endothelium.26 It also helps trigger production of nitric oxide — which improves blood flow and prevents blood clot formation — and significantly reduces oxidative stress in your vascular system, all of which are important to help prevent the development and/or progression of cardiovascular disease. According to Holick, vitamin D deficiency increases your risk of heart attack by 50%, and if you have a heart attack and you’re vitamin D deficient, your risk of dying from that heart attack is virtually guaranteed. Indeed, a Norwegian study27 published in The Journal of Clinical Endocrinology and Metabolism found “a normal intake of vitamin D” significantly reduces your risk of death if you have cardiovascular disease. |
|
Neurological diseases such as Alzheimer’s disease28,29 and epilepsy — In one study,30 epileptics given a one-time megadose of vitamin D3, ranging from 40,000 IUs all the way up to 200,000 IUs, followed by a daily dose of 2,000 to 2,600 IUs a day for three months to bring each individual’s vitamin D status to at least 30 ng/mL, resulted in significant improvements. Ten out of 13 had a decrease in the number of seizures, five of whom experienced more than a 50% reduction. Overall, the group had a 40% reduction in the number of seizures. |
|
Lupus — According to researchers in Cairo,31 most patients with systemic lupus erythematosus have some level of vitamin D deficiency, defined as a level of 10 ng/mL or less, or insufficiency, a level between 10 and 30 ng/mL. |
|
Obstructive sleep apnea — In one study, 98% of patients with sleep apnea had vitamin D deficiency, and the more severe the sleep apnea, the more severe the deficiency.32 |
|
Bone health, falls and fractures — A 2006 review33 looking at vitamin D intakes and health outcomes such as bone mineral density, dental health, risk of falls, fractures and colorectal cancer, found “the most advantageous serum concentrations of 25(OH)D begin at 30 ng/mL, and the best are between 36 to 40 ng/mL.” |
|
Obesity and diabetes — Research34 has shown vitamin D supplementation (4,000 IUs/day) combined with resistance training helps decrease your waist-to-hip ratio, a measurement that is far better at determining your risk for Type 2 diabetes and heart disease than body mass index. |
|
Type 1 diabetes — Data from GrassrootsHealth’s D*Action project to prevent Type 1 diabetes35 suggests maintaining a vitamin D level between 40 and 60 ng/mL (100 to 150 nmol/L) may prevent Type 1 diabetes, and stop the progression of the disease, which is a growing problem. |
|
Neurodegenerative diseases, including Alzheimer’s, Parkinson’s and multiple sclerosis (MS)36 — Research shows MS patients with higher levels of vitamin D tend to experience less disabling symptoms.37 Vitamin D deficiency is also common among patients with Parkinson’s38 and seniors with severe vitamin D deficiency may raise their risk for dementia by 125%.39 |
|
DNA repair and metabolic processes — One of Holick’s studies showed healthy volunteers taking 2,000 IUs of vitamin D per day for a few months upregulated 291 different genes that control up to 80 different metabolic processes, including DNA repair and autoxidation (oxidation that occurs in the presence of oxygen and/or UV radiation, which has implications for aging and cancer). |
|
Preterm birth — A level of 40 ng/mL has also been shown to offer powerful protection against preterm birth if you’re pregnant.40 Women with a vitamin D level of at least 40 ng/mL may lower their risk of preterm birth by as much as 62%, compared to having a level of just 20 ng/mL. Women with a history of preterm birth gain even greater protection — an 80% reduction — when raising their vitamin D level above 40 ng/mL. |
|
Pregnancy complications — Having a vitamin D level above 40 ng/mL also protects the mother by reducing her risk of preeclampsia, gestational diabetes and prenatal infections by approximately 50%.41 |
|
All-cause mortality — Studies have also linked higher vitamin D levels with lowered mortality from all causes.42,43,44 |
Vitamin D Levels Can Affect COVID Risk
Evidence showing vitamin D lowers your risk of SARS-CoV-2 infection, hospitalization, severe complications and death continues to mount, with study after study showing that your vitamin D status before you become infected can greatly affect not only your risk of getting COVID, but how well you recover (or don’t) from it.
Included in those studies is a scientific review45 in the journal Nutrients, which I co-wrote with William Grant, Ph.D., and Dr. Carol Wagner, both of whom are part of the GrassrootsHealth expert vitamin D panel. We found that at least 14 observational studies offer evidence that serum 25-hydroxyvitamin D concentrations are inversely correlated with the incidence or severity of COVID-19.
The evidence to date generally satisfies Hill’s criteria for causality in a biological system, namely, strength of association, consistency, temporality, biological gradient, plausibility (e.g., mechanisms), and coherence, although experimental verification is lacking. Thus, the evidence seems strong enough that people and physicians can use or recommend vitamin D supplements to prevent or treat COVID-19 in light of their safety and wide therapeutic window.
As of October 31, 2021, our paper, “Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity” — which you can download and read for free — was the second most downloaded study from this journal in the previous 12 months. It was also No. 2 in citations and No. 4 for views.
Other studies have also confirmed that higher vitamin D levels lower your risk of complications and death from COVID-19. Among them is an August 2020 study46,47 published in the journal Nutrients, which found patients who had a vitamin D level below 12 ng/mL (30 nmol/L) had a 6.12 times higher risk of severe disease requiring invasive mechanical ventilation, and a 14.7 times higher risk of death compared to those with a vitamin D level above 12 ng/mL.
Other Conditions Affected by Vitamin D Levels
In January 2022 Mayo Clinic research on vitamin D was featured by WEAU 13 News in Wisconsin. The clinic’s list of conditions affected by vitamin D include:48
|
Cognitive health — Research shows that low levels of vitamin D in the blood are associated with cognitive decline. |
|
Inherited bone disorders — Vitamin D supplements can be used to help treat inherited disorders resulting from an inability to absorb or process vitamin D, such as familial hypophosphatemia. |
|
Multiple sclerosis — Research suggests that long-term vitamin D supplementation reduces the risk of multiple sclerosis. |
|
Osteomalacia — Vitamin D supplements are used to treat adults with severe vitamin D deficiency, resulting in loss of bone mineral content, bone pain, muscle weakness and soft bones (osteomalacia). |
|
Osteoporosis — Studies suggest that people who get enough vitamin D and calcium in their diets can slow bone mineral loss, help prevent osteoporosis and reduce bone fractures. Ask your doctor if you need a calcium and vitamin D supplement to prevent or treat osteoporosis. |
|
Psoriasis — Applying vitamin D or a topical preparation that contains a vitamin D compound called calcipotriene to the skin can treat plaque-type psoriasis in some people. |
|
Rickets — This rare condition develops in children with vitamin D deficiency. |
Check Your Vitamin D Level Twice a Year
Regular, sensible sun exposure is the best way to optimize your vitamin D status, but many will need to take an oral vitamin D3 supplement, especially during winter months.
The only way to gauge whether you might need to supplement, and how much, is to get your level tested, ideally twice a year, in the early spring, after the winter, and early fall when you level is at its peak and low point. This is particularly important if you’re pregnant or planning a pregnancy, or if you have cancer.
Again, the level you’re aiming for is between 60 and 80 ng/mL, with 40 ng/mL being the low cutoff point for sufficiency to prevent a wide range of diseases, including cancer.
GrassrootsHealth makes testing easy by offering an inexpensive vitamin D testing kit as part of its consumer-sponsored research. By signing up, you are helping further vital health research that can help millions in coming years. (All revenues from these kits go directly to GrassrootsHealth. I make no profit from these kits and only provide them as a service of convenience to my readers.)
All women are also encouraged to enroll in the Breast Cancer Prevention project,49 to track your vitamin D level and help prevent an initial cancer occurrence, or, if you’ve already had it, to help prevent a recurrence. In addition, anyone affected by Type 1 Diabetes is invited to enroll in the Type 1 Diabetes Prevention Project.
Required Dosage Is Highly Individual
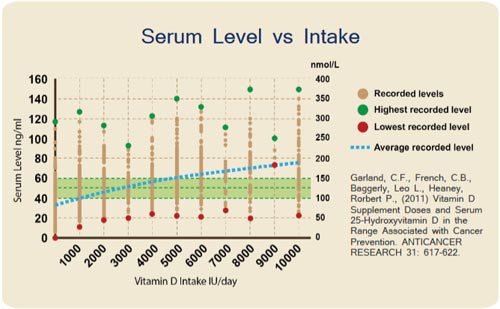
Research50 suggests it would require 9,600 IUs of vitamin D per day to get 97% of the population to reach 40 ng/mL, but individual requirements can vary widely, and you need to take whatever dosage required to get you into the optimal range.
In 2018 I interviewed Carole Baggerly, director and founder of GrassrootsHealth, a nonprofit public health research organization dedicated to moving public health messages regarding vitamin D from research into practice, and she said:
“Our first paper, published in 2011, showed the dose response relationship. You can easily see that two people taking the same dose (e.g., 4,000 IU/day) could have very different results. That’s why testing … is so important.”
If you’ve been taking a certain amount of vitamin D3 for a number of months and retesting reveals you’re still not within the recommended range, then you know you need to increase your dosage.
Over time, with continued testing, you’ll find your individual sweet spot and have a good idea of how much you need to take to maintain an ideal level year-round. GrassrootsHealth also has an online vitamin D calculator you can use to estimate your vitamin D3 dosage once you know your current serum level.
Additional Guidelines When Using Oral Vitamin D3
Aside from determining your ideal dose of vitamin D3, you also need to make sure you’re getting enough vitamin K2 (to avoid complications associated with excessive calcification in your arteries), calcium and magnesium.
Research51,52 has shown that if you’re taking high doses of vitamin D while having an insufficient magnesium level, your body cannot properly utilize the vitamin D you’re taking. The reason for this is because magnesium is required for the actual activation of vitamin D. If your magnesium level is too low, the vitamin D may simply get stored in its inactive form.
This may actually help explain why many need rather high doses of vitamin D to optimize their levels. According to this scientific review, as many as 50% of Americans taking vitamin D supplements may not get significant benefit due to insufficient magnesium levels.
On the other hand, when you have an optimal magnesium level, your vitamin D level will rise even if you’re taking a much lower dose.53 In fact, previous research54 has indicated that higher magnesium intake helps reduce your risk of vitamin D deficiency — likely by activating more of it.