This article was previously published September 7, 2019, and has been updated with new information.
It’s no secret that there are discernible differences in how people respond differently to the same stimuli, especially between men and women. For example, Diane Halpern, Ph.D., past president of the American Psychological Association, wrote an academic text, “Sex Differences in Cognitive Abilities.” Bruce Goldman, science writer at Stanford,1 reported in the preface to the first edition that:2
“At the time, it seemed clear to me that any between-sex differences in thinking abilities were due to socialization practices, artifacts and mistakes in the research, and bias and prejudice … After reviewing a pile of journal articles that stood several feet high and numerous books and book chapters that dwarfed the stack of journal articles … I changed my mind.”
Researchers have also discovered structural differences in the brains of men and women including a larger total brain volume in men and higher tissue density in the left amygdala, hippocampus and insular cortex. Amber Ruigrok, Ph.D., carried out the study revealing the asymmetric effect sex has on a developing brain. She said:3
“For the first time we can look across the vast literature and confirm that brain size and structure are different in males and females. We should no longer ignore sex in neuroscience research, especially when investigating psychiatric conditions that are more prevalent in either males or females.”
As scientists gather more information about the specific differences between men and women, it’s generated numerous questions. Roger Fillingim, Ph.D.,4 from the University of Florida, has spent years researching differences in pain perception and what implications they may have for pain management.5
Women Often Perceive Pain More Intensely Than Men
Fillingim found that differences in personality and behavior associated with gender are quite real and have profound effects on many aspects of life and health. Gender differences affect the ways in which men and women use logic and solve problems. Even while at rest, neurological activities in the brain are different.6
As described in a literature review,7 Fillingim began evaluating an area of research suggesting there are gender-based differences in response to pain. He provided a brief overview of the sex-related differences in biological and sociological processes and the role that sex hormones play in influencing pain sensitivity.
He suggested future directions for research with an emphasis on discovering the mechanisms of difference to assist efforts in prescribing specific treatments for men and women. He participated in a follow-up study8 with the objective of evaluating differences in peripheral and central sensitization in those with symptomatic knee osteoarthritis.
The team concluded there was evidence women have a greater overall sensitivity to pain than men.9 In an interview with NPR, Fillingim explained what has driven his desire to discover gender-based differences in pain perception:10
“The burden of pain is substantially greater for women than men, and that led pain researchers like myself to wonder if the pain perception system is different in women than in men.”
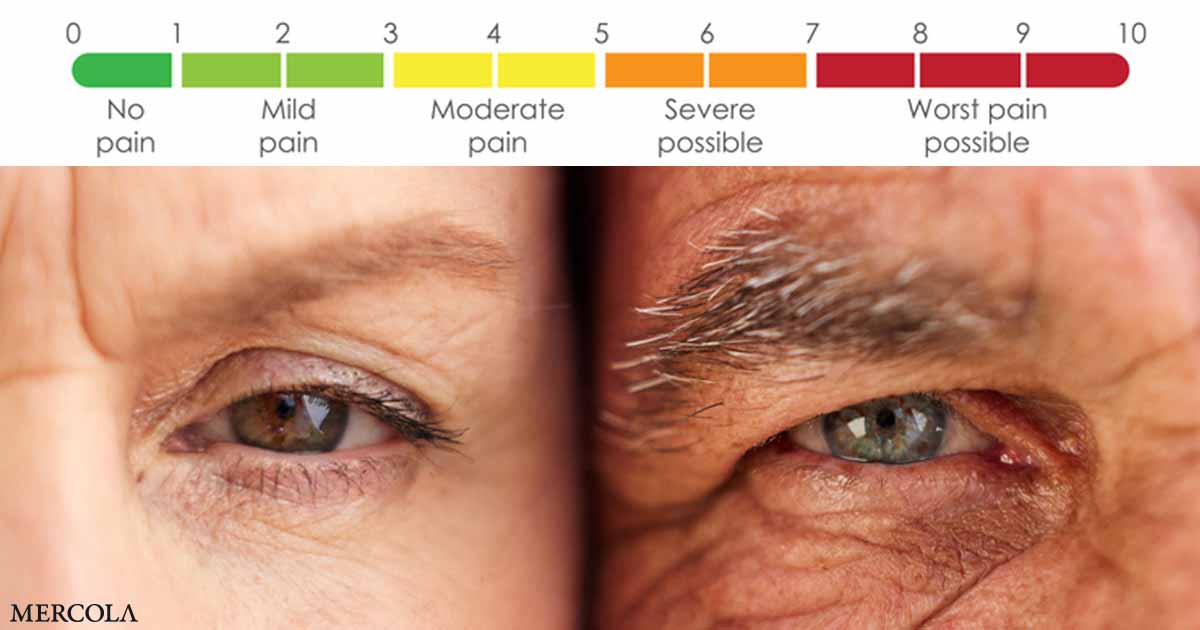
Fillingim is currently the director of the University of Florida’s Pain Research and Intervention Center of Excellence.11 He and his team recruit healthy volunteers for experimental pain sessions during which participants are exposed to painful stimuli in the form of electrical stimulation, pressure, heat or cold.12 The volunteers rate their pain on a standard scale of zero to 10.
Fillingim reported his findings are consistent with those of other researchers.13 While the pain stimuli are the same, women on average report greater pain. Fillingim believes that finding the reason behind the difference may help provide more effective pain treatment beyond a standard prescription for highly addictive opioid drugs.
Pain Perception Is Affected by Several Factors
Fillingim is investigating several factors that influence the perception of pain, including sex hormones. In discussing pain perception of those living with arthritis, scholars from the Arthritis Foundation point out factors influencing perception include age, emotions and support systems.14
In the elderly, regions of the brain that process pain may undergo a structural change predisposing the individual to a reduction in pain perception.15 However, recent studies have shown that sensation may increase or decrease as you age. Psychological state is also a player in pain treatment.
Researchers have found that those who have a negative attitude or emotional state may have an increased intensity of their pain and a poor response to pain control.16 By contrast, those with a positive attitude often experience better clinical treatment of their pain with medication.
In an analysis of chronic pain in individuals, researchers have found that perception is more than just sensation as it often encompasses emotional aspects, the attention of the individual and learned responses over time.17 Anxiety and depression also contribute.
Scientists have found that by providing psychological support they may reduce the use of analgesics and increase an individual’s sense of control. Perceptions in those experiencing chronic pain will also be influenced by their expectation of what they will feel and how they will respond to treatment.18
Based on results of a study Fillingim conducted on those with active knee osteoarthritis, the team suggested that women have an enhanced central sensitivity to pain.19 Central sensitization occurs in the nervous system when an individual experiences chronic pain.20
The condition has two characteristics involving heightened sensitivity, one of which occurs when the person experiences pain under conditions normally not painful. The other occurs when something that is typically painful is perceived as being more painful. In essence, the central nervous system becomes regulated to a persistent state which lowers an individual’s threshold for what causes pain.
What Fillingim found is that the perception of an identical acute pain stimulus is greater in women than in men, and that women also experience an enhanced central sensitization to chronic pain.
More Women Suffer From Anxiety and Pain Than Men
According to Harvard Health Publishing21 there are connections among anxiety, depression and pain. The overlap is particularly significant in those suffering from chronic pain. Researchers are finding that the overlap has something to do with biological mechanisms in addition to psychological factors.
When anxiety and pain overlap, treatment may be challenging. Researchers have found that significant mood disorders apparent before surgical intervention can contribute to the development of chronic pain after surgery.22 One study23 found a link between anxiety and the exacerbation of pain related to the hippocampus, which plays a role in anxiety.24
Anxiety disorders are some of the most prevalent mental health conditions. According to population-based surveys, nearly 33.7% may suffer from anxiety during their lifetime.25 It is important to note researchers have consistently found women suffer from anxiety disorders twice as much as men and that this may be related to life experiences or genetic and neurobiological factors.26
Psychologist Carolyn Mazure, Ph.D., of the Yale School of Medicine27 notes that women are also more likely to have a chronic disability associated with pain.28 The combination of a higher incidence of chronic pain conditions, anxiety disorders and deeper perceptions of pain may greatly contribute to the trend toward the combined use of opioids and benzodiazepines in women.29
Although clinical guidelines caution physicians against this combination, from 2002 to 2014 the proportion of those who received opioids and benzodiazepines together rose from 6.8% to 9.6%.30
Half of those received both drugs from the same physician on the same day; the writing of combined prescriptions was more common in those who were getting opioids for more than 90 days, in both women and the elderly.31
Does Substance Abuse Progress More Quickly?
Drug overdose deaths related to prescription and synthetic opioid use in women jumped significantly from 1999 to 2017.32 The percent increase of total drug overdoses in women ages 30 to 64 years jumped by 260% during that same time.33 Although the number of female deaths was lower than that of males, the number appeared to rise at the same rate until 2017.34
In an analysis35 of a large insurance claims database whose results were published in 2009, researchers studied chronic opioid users and their use of medical services. They found 4.56% of all insurance claims were made by chronic opioid users, who made up just 0.65% of the total population.
Of the group, women represented more than 63% and filed a greater number of insurance claims representing medical services.36 The authors suggest that opioids were often prescribed for arthritis and headaches or at times when patients presented with concurrent physical ailments for which opioids were contraindicated, such as COPD.
Another study37 offers results which are believed to point to gender-based vulnerabilities involving the consequences of addiction in women. The objective was to evaluate the effect of gender on progression from regularly using addictive substances to entering treatment.
The researchers found that women went through fewer years of regular use before choosing to enter treatment; however, they didn’t find a difference in the severity of drug dependence specific to gender.38 They concluded this may support the idea that women go through an accelerated progression of addiction to opioids, cannabis and alcohol.
The study did not address the degree of failure in the participants’ life before seeking treatment. In other words, women may have exhibited a greater understanding of their need for treatment rather than a faster progression through addiction.
Seek Natural Options Before Opioids
If you are struggling with an opioid addiction, please seek professional help immediately. A major step toward healing and health is to make changes to your diet and lifestyle, which may produce significant results. Four primary areas to address include:
- Eliminating or radically reducing your consumption of grains and sugars
- Increasing your intake of animal-based omega-3 fats
- Optimizing your production of vitamin D
- Radically reducing your intake of processed foods
Each of these helps reduce inflammation in your body. If you are fighting chronic pain, it is important to address the underlying issue in order to reduce your discomfort and improve your health. You may find it helpful to start physical therapy or visit a chiropractor to address challenges with posture, lower back pain, chronic headaches or hip and knee pain among others.
In addition to these strategies consider the use of Emotional Freedom Techniques (EFT), which involve psychological acupressure to optimize your emotional and physical health and healing. EFT is easy to learn and may help remove negative emotions, reduce food cravings (including sugar) and reduce pain.
If you are struggling with opioid addiction, EFT may also assist you through a structured recovery program. If you’re currently suffering from chronic pain, you may find comfort knowing there are many natural, safe and effective alternatives you can consider rather than turning to over-the-counter and prescription painkillers.