16th May 2022
Dead eyes brought back to life
Scientists have revived light-sensing neuron cells in organ donor eyes and restored communication between them as part of a series of discoveries that could transform research into the brain-vision system.
Researchers from the John A. Moran Eye Center at the University of Utah and collaborators from Scripps Research in California have described how they used the retina as a model of the central nervous system to investigate how neurons die – and new methods to revive them. Their study is published this month in the peer-reviewed journal Nature.
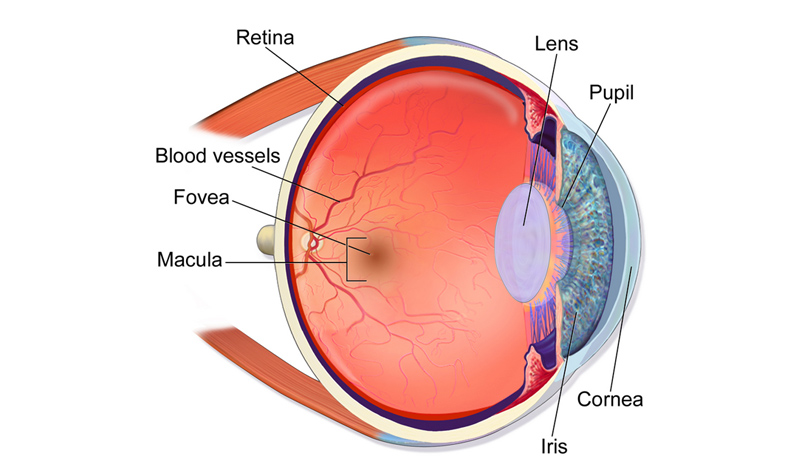
In the brain and central nervous system (CNS), billions of neurons transmit sensory information as electrical signals; while in the eye, specialised neurons called photoreceptors can sense light. It is generally accepted that neurons are irreversibly affected by changes in oxygenation and metabolite supply induced by a stroke or death. The researchers aimed to determine how true this is, using the retina as a model of the CNS.
“We were able to ‘wake up’ photoreceptor cells in the human macula, which is the part of the retina responsible for our central vision and our ability to see fine detail and colour,” explains Fatima Abbas, PhD, Moran Eye Center scientist and lead author of the published study. “In eyes obtained up to five hours after an organ donor’s death, these cells responded to bright light, coloured lights, and even very dim flashes of light.”

Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014”. WikiJournal of Medicine 1 (2).
DOI:10.15347/wjm/2014.010. ISSN 2002-4436., CC BY 3.0, via Wikimedia Commons
While initial experiments revived the photoreceptors, the cells appeared to have lost their ability to communicate with other cells in the retina. The team identified oxygen deprivation as the critical factor leading to this loss of communication.
To overcome the challenge, Scripps Research Associate Professor Anne Hanneken, MD, procured organ donor eyes in under 20 minutes from the time of death, while Moran Eye Center scientist Frans Vinberg, PhD, designed a special transportation unit to restore oxygenation and other nutrients to the organ donor eyes. Vinberg also built a device to stimulate the retina and measure the electrical activity of its cells. With this approach, the team was able to restore a specific electrical signal seen in living eyes, the “b wave.” It is the first b wave recording made from the central retina of postmortem human eyes.
“We were able to make the retinal cells talk to each other, the way they do in the living eye to mediate human vision,” says Vinberg. “Past studies have restored very limited electrical activity in organ donor eyes, but this has never been achieved in the macula, and never to the extent we have now demonstrated.”

The team’s process could be used for studying other neuronal tissues in the central nervous system. It is a transformative technical advance that may lead to a better understanding of neurodegenerative and blinding diseases.
Their study has now generated data from more than 40 human donor eyes – including the first description of a mechanism that is expected to rate-limit the speed of human central vision.
Vinberg notes that this approach can lower research costs compared to non-human primate research and dependence on animal models that produce results that do not always apply to humans. While mice are commonly used in vision research, they do not have a macula. Researchers can also test potential new therapies on functioning human eye cells, speeding drug development.
“The scientific community can now study human vision in ways that just aren’t possible with laboratory animals,” says Vinberg. “We hope this will motivate organ donor societies, organ donors, and eye banks by helping them understand the exciting new possibilities this type of research offers.”

Fatima Abbas, PhD, in the John A. Moran Eye Center at the University of Utah, lead author of the study.
Hanneken, a long-time retinal surgeon, said the ability to produce viable patches of human retinal tissue could lead to new therapies for blinding diseases.
“Until now, it hasn’t been possible to get the cells in all of the different layers of the central retina to communicate with each other the way they normally do in a living retina,” she explained. “Going forward, we’ll be able to use this approach to develop treatments to improve vision and light signalling in eyes with macular diseases, such as age-related macular degeneration.”
This new study joins a growing body of scientific evidence that raises questions about the irreversible nature of death, partly defined by the irreversible loss of neuronal activity. Yale University researchers made headlines in April 2019 when they revived the disembodied brains of pigs, four hours after death, but they did not restore global neuronal activity.
Fast forward a few centuries or millennia. Perhaps by then, our descendants will look back on these experiments in the same way we view the early discoveries of electricity and other phenomena in the 17th-19th centuries. As they read about our primitive understanding of neuroscience and medicine, these future historians will marvel at how death used to always be permanent – before saving the recently deceased became an option.
—
• Follow us on Twitter
• Follow us on Facebook
• Follow us on Instagram
• Join us on Reddit
• Subscribe to us on YouTube
Comments »