By Dr. Mercola
Americans are a pill-popping population, taking an average of 13 different prescription drugs per capita as of last year’s statistics.1 Children in the US are the most medicated in the world, averaging out at four prescriptions per child. Among seniors, drug use is beyond epidemic, averaging out at a staggering 28 prescriptions per person.
The biggest issue is what all of these drugs are really doing to your health.
The facts simply do not support the idea that massive drug use equates to improved health. On the contrary, we’re seeing massive increases in chronic illnesses. As drug use continues to increase, Americans’ health continues to decline, and this is no coincidence… Many drugs actually increase your risk of illness and premature death, and Plavix is just one of many examples.
Plavix and Aspirin – A Most Dangerous Heart Disease Prevention Plan
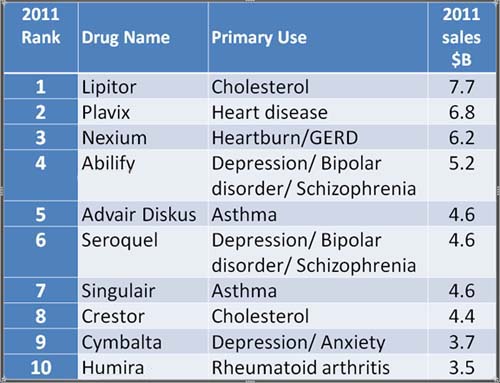
Plavix, manufactured by Bristol-Myers Squibb, is an anti-platelet drug that works by thinning your blood and making it less likely to clot. It is promoted for the prevention of strokes and heart attacks. It’s what is commonly known as a “blockbuster” drug, currently ranking second on the list of top selling drugs of 2011.
Sadly, Plavix also has serious side effects you may not be aware of. Six years ago, I warned my readers that when combined with aspirin, the drug nearly doubled the death rate from heart disease among patients who had not had a previous heart attack but were at risk, compared to those taking aspirin alone.
Plavix Health Risks Confirmed Again
Now, research2 investigating the effects of Plavix in combination with aspirin versus using aspirin alone for the prevention of stroke and cognitive decline has confirmed these disturbing results.
In fact, the anti-platelet arm of the study was terminated3 and patients were told to stop taking Plavix and take aspirin only, as it became apparent the Plavix-aspirin regimen significantly increased the risk of death. The combination also doubled the risk of gastrointestinal bleeding, and more than doubled fatal hemorrhaging. Previous studies have also demonstrated that Plavix patients have a higher rate of stomach ulcers. Numerous lawsuits have been filed by patients alleging they were injured by this common drug.
Here’s something to consider: An aspirin regimen will cost you around $6 per month (or even less than $1 per month if you split regular generic aspirin into quarters), compared to Plavix, which will set you back around $200 per month (or one-tenth of that price if you get generic Clopidogrel).
How in the world can anyone justify the use of a drug that increases your risk of death, and costs 33 to 200 times more than the most common alternative, and to top it all off, call it prevention? It’s really amazing how Bristol-Meyers has managed to pull the wool over everyone’s eyes on this one. Even if you take Plavix alone, without aspirin, you’re still likely wasting huge amounts of money, and, as the new evidence suggests, taking a higher health risk than you would with low-dose aspirin.
A 1996 Lancet study4 comparing Plavix versus aspirin for the prevention of ischaemic events, involving more than 19,000 people followed from one to three years, found that:
“…an intention-to-treat analysis showed that patients treated with clopidogrel had an annual 5.32% risk of ischaemic stroke, myocardial infarction, or vascular death compared with 5.83% with aspirin.”
Note the words “intention-to-treat analysis.” Statistically, when a study uses intention-to-treat analysis, chances are exceptionally great that it has been inadequately applied, “potentially leading to a biased treatment effect,” according to a study5 assessing the methodological quality of intention-to-treat analysis as reported in randomized controlled trials in large medical journals.
What this means in plain English, is that whenever a study resorts to using intention-to-treat analysis, the data has likely been “massaged” in order to achieve a desired result – in this particular case, showing that Plavix was slightly better than aspirin for reducing your risk of stroke, myocardial infarction and vascular death. According to the authors of the above mentioned investigation into the proper methodology of such analysis:
“The intention to treat approach is often inadequately described and inadequately applied. …Readers should critically assess the validity of reported intention-to-treat analyses.”
A Free and Simple Alternative to Plavix
One of the simplest, most inexpensive (as in free), and effective alternatives to blood thinning drugs like Plavix is “Grounding,” also known as “Earthing.” The concept of earthing, was initially developed by Clint Ober. Stated in the simplest terms possible, earthing is simply walking barefoot; grounding your body to the Earth. And before you dismiss this concept as some placebo-induced fantasy by tree hugging hippies, know that at least a dozen scientific papers have been published demonstrating the mechanics and measurable physical effects of grounding.
When you’re grounded there’s a transfer of free electrons from the Earth into your body. And these free electrons are probably the most potent antioxidants known to man. Inflammation is a hallmark of virtually all diseases, so preventing chronic inflammation is key for overall health.
Bare skin in general is a very good conductor. You can connect any part of your skin to the Earth, but if you compare various parts there is one that is especially potent, and that’s right in the middle of the ball of your foot, which is precisely where your foot would strike the ground if you were walking. It’s a well-known point that conductively connects to all of the acupuncture meridians and essentially connects to every nook and cranny of your body. Any free radicals that leak into the healthy tissue will immediately be electrically neutralized. This occurs because the electrons are negative, while the free radicals are positive, so they cancel each other out.
However, there’s more!
Another very important discovery, especially as it relates to grounding as an alternative to blood-thinning drugs, is that grounding thins your blood, making it less viscous – essentially doing the same job that Plavix does, but infinitely safer.
Total Video Length: 32:36
Download Interview Transcript – Part 1
How Grounding Thins Your Blood
Dr. Sinatra has been coaching a team led by Dr. Oschman in how to measure blood viscosity using a method called zeta potential. It measures the potential on your red blood cells by determining how fast they migrate in an electrical field. It turns out that when you ground to the earth, the zeta potential of your red blood cells quickly rises, which means your red blood cells have more charge on their surface, which forces them apart from each other.
This action causes your blood to thin and flow easier. It also causes your blood pressure to drop.
Another obvious implication of this is that by repelling each other, your red blood cells are less inclined to stick together and form a clot. Blood clots don’t have to be very big to form like a pulmonary embolus that would kill you instantly, so this is a significant benefit. Additionally, if your red blood cell’s zeta potential is high, which grounding can facilitate, you not only decrease your heart disease risk but also your risk of multi-infarct dementias, where you start losing brain tissue due to micro-clotting in your brain.
Published in the peer-reviewed Journal of Alternative and Complementary Medicine,6 a recent study into grounding’s effect on blood viscosity found that two hours of grounding increased the surface charge on red blood cells, thereby reducing blood viscosity and clumping. (The full article7 can be viewed for free here.) According to the authors:
“Grounding appears to be one of the simplest and yet most profound interventions for helping reduce cardiovascular risk and cardiovascular events.”
The Best Surfaces for Grounding
Clearly, the simplest way to ground is to walk barefoot outside when safe to do so. But what about urban or city dwellers who are surrounded by asphalt and concrete? Can you ground on those? And what about natural surfaces – which ones are the most effective? There are indeed significant differences between various surfaces. The ideal location for walking barefoot is the beach, close to or in the water, as sea water is a great conductor. Your body also contains mostly water, so it creates a good connection.
A close second would be a grassy area, especially if it’s covered with dew, which is what you’d find if you walk early in the morning. Concrete is a good conductor as long as it hasn’t been sealed. Painted concrete does not allow electrons to pass through very well. Materials like asphalt, wood, and typical insulators like plastic or the soles of your shoes, will not allow electrons to pass through and are not suitable for barefoot grounding.
Chronicle of an Unforetold Death
In 2000, one of the best articles I’ve ever read documenting the tragedy of the traditional medical paradigm was published in the Journal of the American Medical Association (JAMA). The author was Dr. Barbara Starfield of the Johns Hopkins School of Hygiene and Public Health. Based on her article, I created a headline that has reverberated through the web ever since: Doctors Are The Third Leading Cause of Death in the US. Dr. Starfield’s research documented how a staggering 225,000 Americans die from iatrogenic causes, i.e. their death is caused by a physician’s activity, manner, or therapy. Her statistics included the following details:
- 12,000 die annually from unnecessary surgery
- 7,000 die annually from medication errors in hospitals
- 20,000 die annually from other errors in hospitals
- 80,000 die from infections in hospitals, and
- 106,000 die from non-error, negative side effects of drugs each year
Her work opened our eyes to the true state of affairs within our medical system, so it is a truly sad irony that she recently became another statistic of Death by Medicine… In the August issue of Archives for Internal Medicine,8 her husband, Dr. Neil A. Holtzman, MD, MPH writes, in part:
“Writing in sorrow and anger, I express up front my potential conflict of interest in interpreting the facts surrounding the death of my wife, Barbara Starfield, MD, MPH. Within hours after her sudden and unexpected death, I notified the dean of the Johns Hopkins Bloomberg School of Public Health, on whose faculty she served, that Barbara had apparently died of a coronary occlusion… Because she died while swimming alone, an autopsy was required. The immediate cause of death was ‘pool drowning,’ but the underlying condition, ‘cerebral hemorrhage,’ stunned me…
Barbara started taking low-dose aspirin after coronary insufficiency had been diagnosed 3 years before her death, and clopidogrel bisulfate (Plavix) after her right main coronary artery had been stented 6 months after the diagnosis. She reported to the cardiologist that she bruised more easily while taking clopidogrel and bled longer following minor cuts. She had no personal or family history of bleeding tendency or hypertension.
The autopsy findings and the official lack of feedback prompted me to call attention to deficiencies in medical care and clinical research in the United States reified by Barbara’s death and how the deficiencies can be rectified. Ironically, Barbara had written about all of them.”
Drug Safety Must Become a Priority, Not an Afterthought
Dr. Holzman goes on to explain that when a patient dies suddenly (and not while in a health care facility), there’s no routine procedure to notify their physician, even if the patient is autopsied. Therefore, sudden deaths are only in very rare cases ever linked to adverse effects of medical treatment (most common of which is drugs). In this case, Dr. Starfield’s husband personally brought the findings of the autopsy to her doctor’s attention, who subsequently submitted an adverse event report to the FDA, stating that she was receiving Plavix, which may have contributed to her cerebral hemorrhage and subsequent death.
“The report may be the critical action that prompts a modification in use or design of the product, improves the understanding of the safety profile of the drug or device and leads to increased patient safety,” Dr. Holzman writes.
One of Dr. Starfield’s points of contention with the current medical system was the lack of systematic recording and studying of adverse events, and her death highlights this situation, as it is quite possible that it was the Plavix-aspirin combination that killed her, yet if it hadn’t been for an autopsy and her husband insisting on an adverse event report, no one would ever have been the wiser about such a connection.
Dr. Starfield herself pointed out that her statistics were likely far lower than the real count, as they only included people who died in the hospital. They did not include (as there’s no data) people who suddenly die outside a hospital setting, due to a drug side effect.
What if a sufficient number of adverse event reports had been filed prior to her taking a combination therapy of Plavix and aspirin – would her life have been spared? It’s impossible to speculate of course, but what is clear is that someone’s life would eventually be spared if adverse event reporting is taken seriously. Plavix sales brought in $4.6 billion in sales during 2010 alone;9 meanwhile, there’s no telling how many Dr. Starfield’s there are out there, who suddenly collapse and die, and no one is ever made the wiser about their true cause of death…
“As our population ages and morbidities accumulate, the United States needs policies that redirect American medicine to primary care physicians,” Dr. Holzman writes. “By providing continuing care over time, primary care physicians can practice person-focused as opposed to disease-centered care. They can get to know their patients as persons and become aware of their multiple morbidities, alert to the presence or possibility of disease and/or drug interactions.”
…When a specific adverse event is expected (eg, bleeding with clopidogrel), adverse event reporting to FDA should be mandatory, and the manufacturer should be obliged to conduct postmarket surveillance. When a harmful effect is confirmed, the FDA should issue a warning to physicians and require a warning in the package insert. Risks should be weighed against benefits to decide whether the drug should be removed from the market.”
How to Report Adverse Drug Reactions
Only a tiny fraction of all adverse drug reactions are ever reported to the FDA – according to some estimates as little as one percent. In order to truly alert the FDA to a problem with a product they’ve approved, they must be notified – by as many people as possible who believe they have experienced a side effect. This means you can take action against the manufacturers of drugs that continue to put your optimal health at risk, if you feel you have had a bad reaction.
I urge you, if you believe you have experienced side effects from a drug, let the FDA know about it! Please go to the FDA Consumer Complaint Coordinator page, find the phone number listed for your state, and report your adverse reaction.
What to Do if You’re at Risk of Heart Disease
Drugs like Plavix are prescribed as “preventive medicine,” but you can be sure that these drugs will not optimize your health. If you’re at risk for heart disease, I urge you to get your vitamin D levels checked, and if you are deficient, take steps to increase your levels to the therapeutic range of 50-70 ng/ml.
Then simply go through and systematically apply the lifestyle changes described in my Optimal Health Plan. I recently updated it with all the latest guidelines and recommendations, so it’s a really comprehensive health plan, covering everything from diet to stress reduction, exercise and supplements, in a systematic, step-by-step way. Making the proper lifestyle changes will virtually eliminate your risk – sometimes quite rapidly – because it helps to significantly reduce inflammation in your body. And, keeping your inflammation levels low is key if you want to reduce your risk of heart disease. An added boon of applying this program is that it will automatically also help you to prevent and treat type 2 diabetes.