
This article was previously published July 4, 2018, and has been updated with new information.
Thousands of studies have been done on the health effects of vitamin D, and research shows it is involved in the biology of all the cells and tissues in your body, including your immune cells. Your cells actually need the active form of vitamin D to gain access to the genetic blueprints stored inside. This is one of the reasons why vitamin D has the ability to impact such a wide variety of health problems — from fetal development to cancer.
Conventional Vitamin D Recommendations Are Too Low
Unfortunately, despite being easy and inexpensive to address, vitamin D deficiency is an epidemic around the world. A simple mathematical error may also deter many Americans and Canadians from optimizing their vitamin D. The Institute of Medicine (IOM) recommends a mere 600 international units (IUs) of vitamin D per day for adults.
As pointed out in a 2014 paper,1 the IOM actually underestimated the need by a factor of 10 due to a simple mathematical error, which has never been corrected. Moreover, the goal of this recommendation is merely bone health, not optimal health and chronic disease prevention.
Similarly, while the American Medical Association considers 20 nanograms per milliliter (ng/mL) sufficient, a compelling body of research suggests 40 ng/mL is at the low end of sufficiency,2 with 30 ng/mL being the rock bottom for the prevention of common diseases such as heart disease,3 diabetes,4 lung disease5 and more.6,7,8 An ideal level for health and disease prevention is actually between 60 and 80 ng/mL.9
Moreover, according to a study in Anticancer Research,10 it would require 9,600 IUs of vitamin D per day to get a majority (97.5% of the population) to reach 40 ng/mL — a far cry from 600 IUs.
That said, GrassrootsHealth — through its D*Action study — has found a sixfold variability in achieved serum levels,11 meaning one person taking 5,000 IUs of vitamin D per day may achieve a level of just 20 ng/mL while another is able to reach a level of 120 ng/mL taking the same amount. This is why it’s so important to get your vitamin D level tested at regular intervals.
According to data published in the Archives of Internal Medicine,12 75% of American adults and teens are deficient in vitamin D, based on a sufficiency level of 30 ng/mL. If the sufficiency cutoff were to be moved to 40 or 60 ng/mL, deficiency rates in the U.S. would likely be in the high 90% bracket. Even with a sufficiency level of 30 ng/mL, 97% of African-Americans and 90% of Mexican-Americans are deficient in this crucial nutrient.
Most Vitamin D-Deficient People Are at Increased Risk of Cancer
Unfortunately, while many health professionals recommend total sun avoidance to avoid skin cancer, this strategy raises your risk of internal cancers instead — hardly a fair trade! Numerous studies have shown people with higher vitamin D levels have a far lower risk of a wide variety of internal cancers.
Generally speaking, research has shown that once you reach a serum vitamin D level of 40 ng/mL, your risk for cancer diminishes by 67%, compared to having a level of 20 ng/ml or less.13,14,15,16,17,18,19 Research shows most cancers occur in people with a vitamin D blood level between 10 and 40 ng/mL, and the optimal level for cancer protection has been identified as being between 40 and 60 ng/mL.20
Vitamin D also increases your chances of surviving cancer if you do get it,21,22 and this includes melanoma, the most dangerous form of skin cancer.23 There’s also evidence it can improve treatment outcomes. For example, adding vitamin D to the conventional treatment for pancreatic cancer was found to boost the effectiveness of the treatment.24 It also plays a significant part in protecting you from COVID-1925 and protects you from autoimmune diseases.26,27
Vitamin D Deficiency Linked to Colorectal Cancer
In a 2018 study, researchers found an inverse relationship between vitamin D and colorectal cancer,28 which in 2022 is the third leading cancer killer29 in the U.S. The vitamin D levels of 5,700 colorectal cancer patients in the U.S., Europe and Asia were compared to 7,100 cancer-free controls.
Here, a vitamin D level of 12 ng/mL (30 nmol/L) or less was considered a deficiency state; 20 to 25 ng/mL (50 to 62.5 nmol/L) was considered sufficient for bone health. Far higher levels were associated with cancer protection:
- People with a vitamin D level of 12 ng/mL or below had a 31% higher risk for colorectal cancer compared to those with levels between 20 and 25 ng/mL
- Those with levels between 30 and 35 ng/mL had a 19% reduced risk for colorectal cancer
- Those with levels between 35 and 40 ng/mL had a 27% reduced risk
- For each 10 ng/mL increase in circulating vitamin D, the risk for colorectal cancer was reduced by 19% in women and 7% in men
Coauthor Marji L. McCullough commented on the results, saying,30 “This study adds new information that agencies can use when reviewing evidence for vitamin D guidance and suggests that the concentrations recommended for bone health may be lower than would be optimal for colorectal cancer prevention.”
Another study31 published in 2015 found women with vitamin D concentrations of at least 30 ng/mL had a 55% lower risk of colorectal cancer than those who had a blood level below 18 ng/mL. And, a 2019 study showed that high-dose vitamin D benefits patients with advanced metastatic colorectal cancer.32
Vitamin D Protects Against Breast Cancer
Several studies also show that higher vitamin D levels are protective against breast cancer specifically, which is a serious concern for most women. For example, in a 2005 study,33 women with vitamin D levels above 60 ng/mL had an 83% lower risk of breast cancer than those below 20 ng/mL.
More recently, a pooled analysis of two randomized trials and a prospective cohort study again confirmed the link between vitamin D and breast cancer risk.34
The objective was to assess whether there are any benefits to having a vitamin D level above 40 ng/mL, as most studies do not venture into these higher levels. Indeed, mirroring the 2005 findings, women with vitamin D levels at or above 60 ng/mL had an 82% lower incidence rate of breast cancer than those with levels of 20 ng/mL or less.
Pooled data was analyzed in three different ways. First, incidence rates were compared based on vitamin D levels ranging from 20 to 60 ng/mL. Next, statistical analysis using Kaplan-Meier plots were done. Third, multivariate Cox regression was used to examine the association between various vitamin D levels and breast cancer risk. According to the authors:
“Results were similar for the three analyses. First, comparing incidence rates, there was an 82% lower incidence rate of breast cancer for women with 25(OH)D concentrations ≥60 vs <20 ng/mL.
Second, Kaplan-Meier curves for concentrations of <20, 20–39, 40–59 and ≥60 ng/mL were significantly different, with the highest proportion breast cancer-free in the ≥60 ng/ml group (99.3%) and the lowest proportion breast cancer-free in the <20 ng/ml group (96.8%). The proportion with breast cancer was 78% lower for ≥60 vs <20 ng/mL.
Third, multivariate Cox regression revealed that women with 25(OH)D concentrations ≥60 ng/ml had an 80% lower risk of breast cancer than women with concentrations <20 ng/mL, adjusting for age, BMI, smoking status, calcium supplement intake, and study of origin … Higher 25(OH)D concentrations were associated with a dose-response decrease in breast cancer risk with concentrations ≥60 ng/mL being most protective.”

Vitamin D Deficiency Linked to Lung Disease
Other recent research35 links vitamin D deficiency to interstitial lung disease (ILD). Here, the vitamin D levels of more than 6,300 individuals of various ethnicities were assessed to evaluate the connection between vitamin D and ILD prevalence and progression. Thirty-three percent had a vitamin D level at or above 30 ng/mL; 35% had levels between 20 and 30 ng/mL and 32% were deficient, having a level at or below 20 ng/mL. According to the authors:
“Compared with those with replete concentrations [at or above 30 ng/mL], participants with 25(OH)D deficiency had greater adjusted high-attenuation areas volume at baseline and increased progression over a median of 4.3 years of follow-up. 25(OH)D deficiency was also associated with increased prevalence of interstitial lung abnormalities 10 years later …
Vitamin D deficiency is independently associated with subclinical ILD and its progression, based on both increased high-attenuation areas and interstitial lung abnormalities, in a community-based population. Further studies are needed to examine whether vitamin D repletion can prevent ILD or slow its progression.”
Even when taking other factors into account, such as age, smoking, obesity and inactivity, the results held true. Dr. Erin Michos, associate professor of medicine at Johns Hopkins University School of Medicine and lead author of the study told Medical News Today:36
“We knew that the activated vitamin D hormone has anti-inflammatory properties and helps regulate the immune system, which goes awry in ILD. There was also evidence in the literature that vitamin D plays a role in obstructive lung diseases such as asthma and [chronic obstructive pulmonary disease], and we now found that the association exists with this scarring form of lung disease too.
We might now consider adding vitamin D deficiency to the list of factors involved in disease processes, along with the known ILD risk factors such as environmental toxins and smoking.”
Vitamin D Deficiency Linked to Pregnancy Loss
Vitamin D is perhaps particularly crucial for pregnant women, to protect both their health and the health of their babies. Interestingly, recent research37,38 suggests vitamin D plays an important role in preventing an adverse immune response against the fetus that might cause her body to reject it as foreign tissue.
As noted by the authors, “It stands to reason that an immunocompetent mother would muster an immune response against the fetus. Nevertheless, in reality this does not occur due to various fetomaternal interactions which induce tolerance … Recently, it has come to light that vitamin D may play an integral part in the induction and regulation of this critical immune tolerance process.”
What they discovered is that recurrent pregnancy loss, which affects about 1% of couples trying to conceive, is linked to low vitamin D. In short, vitamin D promotes a favorable environment for pregnancy, in part by regulating immune cell differentiation and the excretion of inflammatory cytokines.
According to the authors, “It seems that vitamin D deficiency sways the balance toward a worse outcome and may play a part in recurrent pregnancy loss.” Vitamin D also performs many other important functions during pregnancy, and has been shown to dramatically lower a woman’s risk for complications and premature birth.
Vitamin D Significantly Lowers Risk of Preterm Birth
According to findings by Grassrootshealth, there’s a clear and definitive correlation between vitamin D levels and time of gestation — up to 40 ng/mL, where the impact plateaus.39
Overall, evidence shows pregnant women with a vitamin D level between 40 and 60 ng/mL have 46% lower preterm birth rate than the general population, while those with a vitamin D level at or above 40 ng/mL by their third trimester have a 59% lower risk for premature birth compared to those with levels below 20 ng/mL.40
Among non-Caucasian women (among whom vitamin D deficiency is far more common) the reduction in risk is even more significant. In this group, those who achieved a vitamin D level of 40 ng/mL by their second vitamin D test had a 78% lower preterm birth rate — reducing the preterm birth rate from 18% to 4%! To ignore this astounding improvement in preterm birth rate among African-American would be foolhardy in the extreme.
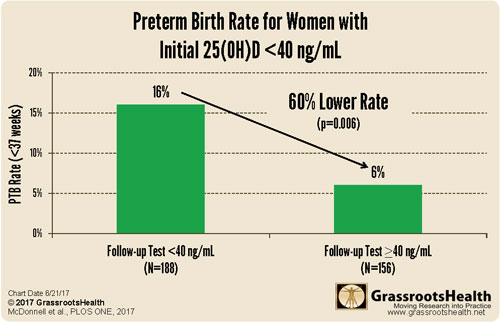
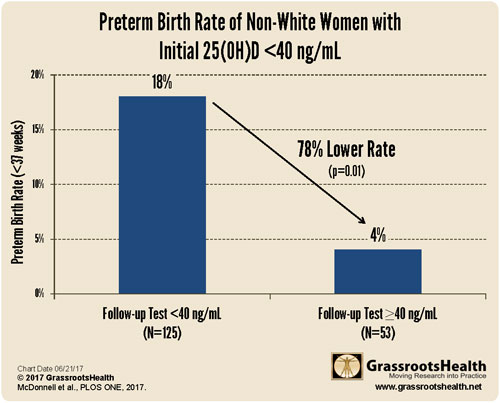
As noted in a 2015 press release announcing the findings:41
“The March of Dimes estimates that the annual cost of preterm births in the United States as $12 billion (for 455,918 children). If approximately 50% of preterm births could be prevented in the general population, as this analysis suggests is possible, there could be $6 billion available for other services, and more than 225,000 children and families spared this trauma.”
What’s more, further analysis revealed that women with a history of preterm birth can lower their risk by a whopping 80% by raising their vitamin D level above 40 ng/mL.42 Tragically, despite the overwhelming evidence43 supporting the use of vitamin D to dramatically improve pregnancy outcomes and lower preterm birth rates, health authorities still make no mention of it whatsoever.
On March 27, 2018, in an effort to break the silence, the Organic & Natural Health Association submitted a health claim petition for vitamin D and preterm birth to the U.S. Food and Drug Administration,44 the key message being that vitamin D supplementation “directly impacts health outcomes and is changing the standards of care, in this case, for pregnant women and a generation of children.”